Last updated on October 20th, 2022 at 01:25 pm
It came on quickly and out of nowhere. Wednesday morning Shelby woke with a little runny nose, nothing to worry about. Later in the afternoon, however, as I was holding her I noticed a faint wheezing sound. It was so quiet I had to put my ear right up to her little body to hear it. Although I’m a new mother to 9-month-old fraternal twins, I understood that wheezing coming from a baby is never a good thing. I immediately called the pediatrician just in time to catch their automated message reminding me that they close at noon on Wednesdays. CRAP.

Luckily, our pediatrician is amazing and responds to emails fairly quickly. She explained that we should take Shelby to urgent care if the wheezing got worse, or if she had a “coughing fit.” At this point, Shelby seemed okay, but was working hard to breathe. Her body moved in and out with each quick breath, and the wheezing continued. I began to call my insurance company to find out which urgent care was in network, and after several calls and about 30 min on hold; I finally got the information I needed. I texted my husband to meet me there and I packed up the babies. When we arrived at urgent care, we were seen by a doctor (after lots of waiting of course) who told us that Shelby’s wheezing was coming from her nose. Her lungs were all clear. And so we went home.
The next morning her wheezing continued, along with congestion and coughing. My gut told me that something wasn’t right. I called the pediatrician the moment they opened and got the first appointment. The pediatrician listened to her lungs for 2 seconds then looked up at me and said, “She’s definitely wheezing and she’s very sick.” What?!! How could the doctor at urgent care miss this? What if I had trusted her judgment and didn’t bring Shelby in to get our doctor’s opinion?? Her diagnosis was either RSV or Bronchiolitis. The pediatrician suggested that we try to treat this at home, and she sent us off with an inhaler (Albuterol) and a decongestant.

We were home about 5 hours when I realized the inhaler treatments were not working, and she was actually getting worse. She was working hard to breathe and wheezing loudly. As I watched her struggle, I began to map out my plan. I texted my husband, asking him to come home from work. Alice was still napping, so I held Shelby as I called the pediatrician. While I was on hold with the pediatrician, I walked across the street to the neighbor’s house and asked her to come sit at the house with Alice so we could go to the ER. I texted a good family friend who lives in the neighborhood, and asked her to come to the house to be with Alice. Even though I was worried about my baby, I felt strangely calm.
The 25 minute drive to the ER felt like hours, and the experience was not what I expected. I imagined running into the ER, kicking the doors open, and screaming, “Somebody help my baby!” In reality, the emergency room has a system. It has rules. Blah. I had to sign in, answer questions, and wait. We waited 20 minutes as I paced the small room. All eyes were on me as I tried to comfort a screaming, naked baby. When we finally got taken back, I felt a little relief. If things got really bad, I knew they could help her.
We spent about 8 long hours in a tiny room in the ER. Here they monitored Shelby’s vitals, gave her a breathing treatment (Xoponex), gave her oxygen, completed a chest x-ray, took blood, attempted to insert an IV for antibiotics and fluids, then tried unsuccessfully again until I asked them to stop. Here my husband and I helped to hold our screaming baby still while a room full of people attempted to find a vein. Here time slows down and you begin understand the utterly helpless feeling of not being able to comfort your baby. Here you tell yourself this is what she needs to get better, and it will be over soon. Here is where the journey really began.

Around 11:30 pm we were moved up to the pediatric floor into a room with two other families. This means two other coughing and fussing babies, two other sets of parents, 3 different TVs blaring, and nurses bumping into things as they tried to move around 3 beds and lots of loud beeping equipment. In this room we waited about 30 minutes for a NICU nurse to become available to help with the IV insertion. Starving, tired, scared, and exhausted, we waited in the small crowded room. My husband went with Shelby to the “treatment room” for the IV insertion and catheter for a urine sample. While I listened to my baby’s tortured screams down the hall for what felt like an eternity, I began to boil. I was pissed that it was taking them this long to get her IV in. I was pissed that I had to stand here helpless listening to her scream, like I had never heard her scream before. I was pissed that we were stuck in a room full of sick babies. I was tired. I was mad that we were back in this hospital after my own 6 weeks of hospitalized bed rest and 3 weeks in the NICU with the babies.
I used my anger to advocate for my baby’s health and make demands. I told the nurse that we couldn’t stay in this room. Clearly it was so crowded that we couldn’t even reach our baby in her crib. After they finally got the IV in, and after 3 negative RSV tests, they moved us to another room with only one other baby. Here, I had to demand that the nurse use Xoponex for a breathing treatment instead of Albuterol (which didn’t work), even if that meant calling the doctor for approval. “It’s not on the orders,” she said. Are you kidding me right now?!! Call the doctor and get it approved. I don’t care if it’s almost 2am. Why is everything taking so long? My baby needs a breathing treatment and we are waiting for a respiratory therapist to be available?? EVERYTHING happens slowly in the hospital. I was melting down.

With one small couch available for sleeping, my husband urged me to go home. Just thinking about leaving Shelby made me want to cry, but I trusted my husband to take charge while I was gone. I drove home around 2 am to relieve our babysitting friend, and then went back to the hospital first thing in the morning after my mom arrived to stay with Alice. When I got to the hospital, Shelby was struggling and working hard to breathe. Soon they decided she would be better off in the pediatric ICU and started prepping her to leave. My heart fell. Oh my g-d, the ICU. Things were getting worse, and as all of these strangers tended to my sick baby I felt so out of control.
Things were chaotic when we arrived in the ICU. Nurses and doctors surrounded Shelby doing a dreadful thing called “deep suction” that made her scream in between gagging. It was awful, and they continued to do this throughout the next few days. After several hours in the ICU, she began to slowly improve. Over the next few days, she became more and more alert and less lethargic. She managed to last longer than 3 hours between breathing treatments, and gradually went every 6 hours without needing help to breathe. Her follow up x-ray proved that it was not pneumonia, but bronchiolitis like our pediatrician predicted.

Days are strange and long inside a hospital. Time chugs away slowly, interrupted by vital checks, breathing treatments, medications, an unhappy baby, and beeping machines. There’s not much difference between day and night inside a hospital. Nurses have shift changes and the lights are a little dimmer, but everything carries on just the same is it does during the day. Vitals are checked, alarms beep, the respiratory therapist comes in and out of the room, a tired and sick baby demands a bottle every time she is woken up. The long sleepless night stretches into a new day, where it all continues again. For our sanity, and for time at home with Alice, my husband and I stayed with Shelby in shifts. As we swapped shifts, we briefed each other on each baby. We talked bottles, naps, medications, breathing treatments, deep suctions, pulse ox. It was lonely, strenuous, exhausting, and a little scary, but as Shelby showed signs of improvement, things felt more tolerable.
After 3 days in the PICU, Shelby moved back up to pediatrics. The goal here was to remain off of oxygen for 24 hours. In the beginning, she would desaturate during sleep, but eventually she was able to sleep without oxygen. On day 6 of our hospital stay, Shelby was discharged. Shelby and Alice were reunited in front of the hospital (which was much less dramatic and adorable than I thought it would be), and we all drove home as a family.

Things like this are supposed to make you stronger, and I guess they do. But they also show you a glimpse of how terrifying things can get when something goes wrong. They show you how swiftly things can change, how awful it feels to watch your baby struggle.
Thank G-d Shelby is okay and improved so quickly. I’m so lucky to have a strong and devoted husband that remained calm and present through the whole experience. I’m so lucky to have family that stepped in to help take care of Alice at home. I’m so lucky that my “mom intuition” (however new it is) drove me to trust my instinct and act quickly. If something like this happens again, I will understand the signs, be thoroughly prepared, and trust my instincts. Weeks later, I am just now beginning to recover (emotionally and physically) and to feel more rested and at ease.
Motherhood is an incredible experience, full of this (twin) love that tugs at my heart and makes me feel like I’ve never felt before. Everything is for these babies.
“Making the decision to have a child – it is momentous. It is to decide forever to have your heart go walking around outside your body. ” ― Elizabeth Stone
Twiniversity Notes on Respiratory Distress

Breathing problems in children should be taken VERY seriously. If you believe your child is under distress, call your pediatrician immediately or head straight to the ER. You can call your pediatrician on your way to the ER and ask them to call the ER to let them know you are coming, which will help the ER prep for your arrival. Do not hesitate to call an ambulance if you fear your child is under severe distress — that is the fastest way to get your child the critical help they need. Never second guess your gut instinct!
Also note that if your child is prone to breathing problems every time they get a cold, request an at-home nebulizer (breathing treatment machine) from your pediatrician. Most health insurance companies will cover this cost and it will save you trips to the ER if you can try to settle the breathing issues at home, because it’s often the same medication they would get in the ER. Talk to your pediatrician for more information.
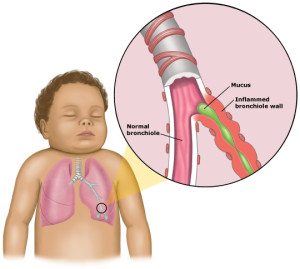 Signs of Bronchiolitis
Signs of Bronchiolitis
For the first few days, the signs and symptoms of bronchiolitis are similar to those of a common cold:
- Runny nose
- Stuffy nose
- Cough
- Slight fever (not always present)
After this, there may be a week or more of breathing difficulty or a whistling noise when breathing out (wheezing). Many infants will also have an ear infection (otitis media).
When to see a doctor
If it’s difficult to get your child to eat and his or her breathing becomes more rapid or labored, contact your child’s doctor. This is especially true if your child is younger than 12 weeks old or has other risk factors for bronchiolitis — including premature birth or a heart or lung condition.
The following signs and symptoms are reasons to seek prompt medical attention:
- Vomiting
- Breathing very fast — more than 60 breaths a minute — and shallowly
- Skin turning blue, especially the lips and fingernails (cyanosis)
- Lethargy
- Refusal to drink enough fluids, or breathing too fast to eat or drink
- Audible wheezing sounds
- Ribs seem to suck inward when infant inhales
Credit: MayoClinic.org

Rachel Brehm, mother to 7-month-old fraternal twin girls, blogs regularly on eating disorder awareness and insurance denials for eating disorder treatment. Brehm writes for an Insurance Law Blog as well as an Eating Disorder Law Blog (rated as one of Top 25 Eating Disorder Blogs of 2012) focusing her writing on insurance advocacy, insurance coverage, body image, eating disorder recovery, and weight stigma. As a new contributor to Twiniversity.com, Brehm plans to shift her writing on body image issues in the insurance world to include body image issues in the mommy world. Brehm’s writing will address navigating pregnancy and postpartum with eating/body image issues as well as her experiences raising twin girls-and all the “twin moments” that go along with it. For more posts by Rachel on Twiniversity, click here.